Engaging the Private Sector in Kinshasa to Strengthen Routine Immunization Service Delivery and Improve Equity
October 31st, 2019 | viewpoint
Strengthening routine immunization in urban settings requires collaboration across partners, including with the private sector. To address this, JSI has been working with the Expanded Programme on Immunization (EPI) and partners in the Democratic Republic of Congo (DRC).
Rapid urbanization has challenged immunization programs and led to inequities in access and utilization of vaccination and health services, resulting in larger numbers of children not completing the recommended vaccination schedule. In large urban settings with high rates of migration, this presents an imminent threat of disease outbreaks like measles as well as risks for other disease transmission and regional/global health security, such as Ebola virus.

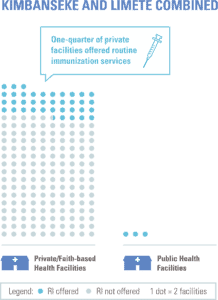
As part of JSI’s ongoing efforts to improve immunization equity, JSI conducted a situational analysis in June 2018 in two health zones of Kinshasa – Limete and Kimbanseke – to analyze bottlenecks and challenges facing urban populations, specifically access and utilization of routine immunization services by urban poor communities. A key finding from this assessment was that while private and faith-based health facilities (HFs) significantly outnumbered governmental facilities, only about one-quarter of such facilities offered routine immunization services[1]. Although some private health providers in DRC already provide immunization services, this number needs to be increased to reach all eligible children and pregnant women.
 Another challenge identified was in regulating the quality of immunization services at private health facilities, as they are not included in standardized EPI training and capacity building activities. Monitoring and management of vaccine storage are similarly unregulated due to the public-private divide. The EPI, therefore, has limited insight into vaccination at private health facilities, as they are not included in administrative health reporting mechanisms. This intensifies the opaqueness of denominator estimations for urban populations in Kinshasa and the country as a whole.
Another challenge identified was in regulating the quality of immunization services at private health facilities, as they are not included in standardized EPI training and capacity building activities. Monitoring and management of vaccine storage are similarly unregulated due to the public-private divide. The EPI, therefore, has limited insight into vaccination at private health facilities, as they are not included in administrative health reporting mechanisms. This intensifies the opaqueness of denominator estimations for urban populations in Kinshasa and the country as a whole.
These challenges affect vaccine forecasting and planning of immunization activities which ensure that all children are reached. Additionally, the analysis found that while immunization services are free in all facilities, some caregivers are being charged for the child vaccination cards. These home-based records are required for documenting a child’s vaccination doses and ensuring a reduction in missed opportunities for vaccination; however, the financial barrier imposed is a significant deterrent to most caregivers.
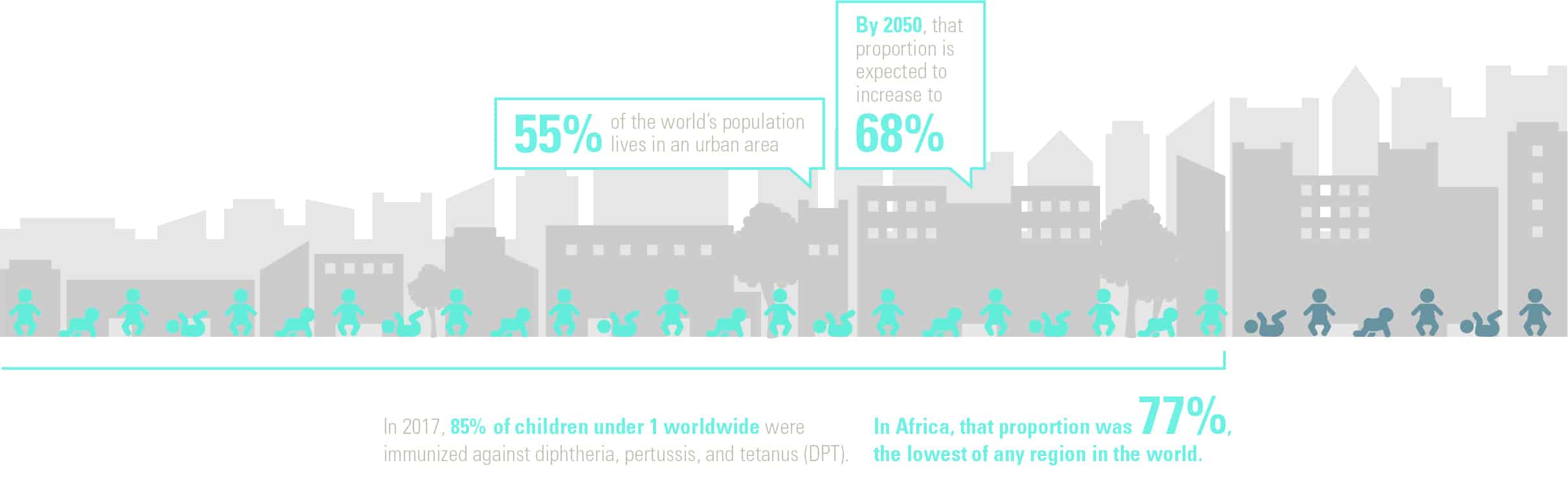
Exploring how to reach dense urban areas such as Kinshasa with sustainable immunization services is crucial. Today, 55 percent of the world’s population lives in an urban area; by 2050, that proportion is expected to increase to 68 percent. Almost 90 percent of that increase is expected to be in Asia and Africa. Urbanization can make the challenge of delivering routine immunization services even more difficult.
Urbanization often brings unplanned growth, poor health infrastructure, de-prioritization of preventive care, few well-being services, poor housing conditions, and poor access to both sanitation and clean drinking water. Urban poor populations, especially infants and young children, are at a higher risk of contracting infectious diseases and exposure to outbreaks, experience high incidence of diarrheal diseases, malnutrition, and mortality due to the lack of appropriate health care.
Currently, it is estimated that immunization saves the lives of 3 million children a year but 2 million more lives could be saved by existing vaccines. In 2017, 85 percent of children under 1 worldwide were immunized against diphtheria, pertussis, and tetanus (DPT). In Africa, that proportion was 77 percent, the lowest of any region in the world.
 Kinshasa is central to Africa’s largest and fastest-growing urban system. By 2030, it is expected to grow to 24 million and be the most populous city in Africa. The challenges of immunization in an urban context are evident in Kinshasa, and for this reason, it is a central part of EPI programming, including the Emergency Plan for the Revitalisation of Routine Immunisation in the DRC (or, Mashako Plan). Since 1997, internal conflict and rural-urban migration for employment opportunities have accelerated the pace of urbanization in the country; more than half of the country’s population is estimated to be urban residents (as of 2018)[2].
Kinshasa is central to Africa’s largest and fastest-growing urban system. By 2030, it is expected to grow to 24 million and be the most populous city in Africa. The challenges of immunization in an urban context are evident in Kinshasa, and for this reason, it is a central part of EPI programming, including the Emergency Plan for the Revitalisation of Routine Immunisation in the DRC (or, Mashako Plan). Since 1997, internal conflict and rural-urban migration for employment opportunities have accelerated the pace of urbanization in the country; more than half of the country’s population is estimated to be urban residents (as of 2018)[2].
DRC’s Path to Immunization Equity
JSI, in collaboration with the EPI and stakeholders, developed practical and actionable strategies for improving routine immunization equity in response to the situational analysis findings. Some examples of strategies to strengthen private sector engagement, currently being implemented with technical support from JSI, include:
As part of implementation research, JSI is documenting the impact of these and other strategies on improvements in urban immunization service delivery, reduction in missed opportunities for vaccination, increase in the number of children vaccinated and other measures of immunization equity. Promising interventions are being proposed for scale in all Health Zones of Kinshasa and to the 11 other major metropolitan centers in the DRC, as part of the country’s Mashako Plan.
Targeted strategies like these are needed to address the inequities that arise through increasing rapid urbanization. It is important to note, however, that there is no one-size-fits-all solution. Each urban context will have a unique set of strategies to meet the needs of its urban populations, given other country priorities, resources, challenges, and opportunities. Tailored immunization technical support is therefore beneficial for capacity transfer and sustainability.
1- Routine immunization refers to the provision of all vaccines required to be fully immunized against vaccine-preventable diseases, according to the country’s vaccination schedule.
2- United Nations, Department of Economic and Social Affairs, Population Division (2018). World Urbanization Prospects: The 2018 Revision, custom data acquired via website.
Written by Michel Othepa and Chloe Manchester
We strive to build lasting relationships to produce better health outcomes for all.