Reaching the Unreached: How self-testing is improving male uptake of HIV services
November 24th, 2020 | story
“The people attending us talk sarcastically…”
“They look at us like we have committed a crime…”
“If I am found HIV-positive, I will become a laughing stock in the community…”
These are just some of the reasons that men in Zambia are reluctant to access HIV services at clinics. But as the country edges toward HIV epidemic control, this key gap must be filled: find out-of-care men who have HIV and provide them with services.
In 2016, the USAID DISCOVER-Health project conducted a study of male sexual partners of adolescent and young women (the Male Characterization Study, or MCS) and heard about the stigmatizing treatment above. Fear and apprehension leave men to delay services until they are so sick that they have no choice.
Josephine Namwila is an antiretroviral therapy (ART) nurse based at St Luke’s Clinic in Lusaka’s Kuku Compound. She offers another reason why men don’t visit the clinic. “I think the main barrier is their mentality. They say that clinics are for women, not for men. Usually what happens is when they come, they find women are the majority here, like today.”

In June 2020 during Child Health Week, the waiting room was filled with women talking, small children playing, and babies wailing, visually and audibly demonstrating Josephine’s point. She says it’s not as simple as a gender divide, though. “It’s also to do with time. Men are busy. They are the breadwinners. Their wives are at home; they have to go out every day to look for money to feed the family. They don’t have time to come to the clinic.” This concurs with what the men told us in the study: coming to busy clinics to line up with women and children for services carries a strong social stigma, in addition to the potential wage loss. So men, unless very sick, simply stay away.
In response to these challenges, the project, in addition to other measures, embarked upon a community-level HIV self-testing effort in December 2018. Josephine explains the approach: “We are going to them in the places where they are, like bus stations and markets. We do outreach to follow them and offer services like HIV self-testing. We go twice a week to the hotspots and run a men’s clinic on Saturdays and Sundays.”
The self-testing option has increased service access and use, Josephine says.
Sometimes these men are scared of a small prick. With the self-test they are more confident.”
The clinic-based test involves a prick on the finger to take blood and must be done by a health professional; the self-test is a swab from the inside of the gum that clients can do themselves at home. Results take about 10 minutes; those who get a reactive (positive) result must come to a clinic for a confirmation test.
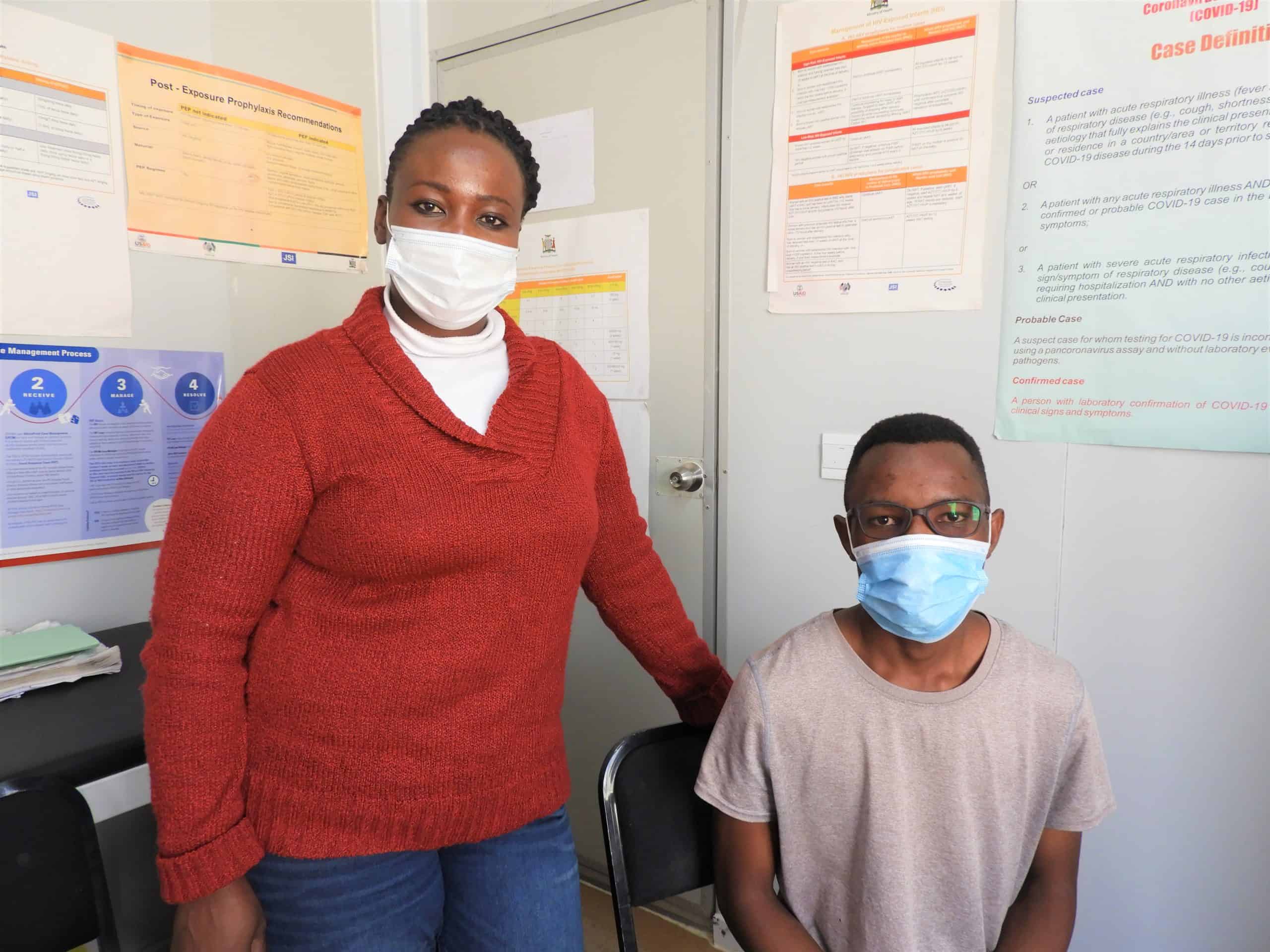
Since the project began the self-testing effort, uptake has been impressive. Between October 2019-September 2020, 21,235 people accessed HIV self-testing across all project sites, including St Luke’s, where Queen Macha is a community mobilization officer. “My job is, I go out in the community to mobilize people, specifically men…we explain the benefits of being tested. I love interacting with different people…and helping those in need.”

During a mobilization effort in February 2020, Queen met Davies, who is 22 and lives in Lusaka with his mother. Davies was playing football with his friends when they noticed brightly colored tents and people gathering. “I saw counselors doing outdoor HIV testing, like an outreach program. So my friends and I decided to go for it! I was pretty nervous actually but with my friends there I felt a bit braver.”
In a private space in the tent, Queen explained how the self-test worked, possible outcomes, and the treatment and prevention options available. Davies took the test and waited for the result. “Unfortunately, it was positive,” he says. “At first, I couldn’t believe it. I didn’t have the slightest idea where I could have got it, or how it came about. When my friends asked me about my results, I kept it from them. I just said it was ok. I really didn’t know how to say it.”
Queen and Davies exchanged contact information, and Queen promised to be in touch. Davies describes the shock he felt on returning home that day. “It was pretty bad. I was scared. I was thinking, how am I going to tell my mum? Even the person I was dating. I was thinking, maybe she’s infected as well? I thought that was it for me. I thought no one would accept me.”
As promised, Queen followed up and encouraged Davies to come to the clinic. He recalls, “I needed to find the courage to face up to reality. Queen brought me to the facility. I was counseled again and then able to tell my mum. She was shocked but she helped me and she supports me. And my girlfriend too. Luckily, she tested negative. I felt even more love, with everyone supporting me.”
In March, Davies started ART. “At first, I didn’t deal with the whole thing of taking medicine very well,” but he’s seen improvements and is happy with his progress: “I’m even getting there with suppressing my viral load!”
Between October 2019 and September 2020, DISCOVER-Health’s community mobilization program helped 93,935 men like Davies access HIV testing. Of those, 7,959 were found to be HIV positive; 7,970 of those men initiated ART.
In addition to DISCOVER-Health’s efforts, positive peer influence, strong family support systems, and helpful provider attitudes are significant facilitators of service uptake for men. Josephine is pleased with the results her team is seeing. “We give men the information and we offer the services. For those that fail to come we make follow-ups. We deliver drugs to them or take samples for self-testing. Of late, we’ve seen a big positive change. Men are now coming [to the clinic]!”
We strive to build lasting relationships to produce better health outcomes for all.