Using Quality Data to Improve Health Service Outcomes
July 14th, 2021 | story
Amal Amhed, director of Jinella Health Center
The Jinella Health Center serves nearly 30,000 residents of the city of Harar in the Harari National Regional State, Ethiopia. Recently, it was lauded for its response to a typhus outbreak and increasing malaria cases. With the help of the Ethiopia Data Use Partnership (DUP), a joint initiative of JSI and the Ministry of Health (MOH), the center has improved its data quality and use of high-quality health information, empowering a practice of evidence-based decision-making.
“It was the all-time record high.”
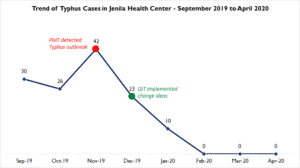
In November 2019, Jinella’s performance monitoring team (PMT) noticed a surge in typhus cases. Reports indicated that cases had increased from 30 to 42 in two months. “It was the all-time record high for our health center. We found it very alarming and it needed to be addressed urgently,” says Amal Ahmed, director of the center and PMT chairperson.
Jinella quickly deemed the typhus outbreak a public health emergency and formed a quality improvement (QI) team within the PMT to determine the source of the outbreak and to map and implement interventions. With this hefty assignment, the QI team worked tirelessly, reviewing piles of records and a plethora of data to discern the leading cause of the outbreak. As part of its approach, the QI team applied the information use cycle, a process to improve performance adopted by Ethiopia’s Ministry of Health (MOH) that involves identifying gaps; prioritizing problems; investigating root causes; and recommending and implementing interventions.
“The team traced the data to Bote Area, a street where homeless people dwell in the city of Harar,” says Haregawin Hailu, health information technology expert at Jinella and QI team member. Not only did the team’s meticulous efforts lead to the identification of the initial location of the outbreak, they also found that the lack of access to proper hygiene and sanitation services were its root causes. The QI team recommended sanitizing the area, making facilities accessible, and providing fresh clothes to the people who dwelled there. The team also said that these citizens’ access to services and facilities would need to be maintained to further contain the typhus’ spread.
However, these recommendations—especially providing permanent access to sanitation and hygiene services—seemed impossible due to scarce resources and limited capacity. So Jinella launched a resource mobilization campaign that yielded various sanitation and hygiene items, including soap and clean clothes, from the Harari Regional Health Bureau (RHB), local partners, and community members.
In December 2019, following the resource mobilization, Jinella organized a week-long campaign to implement the QI team’s recommendations. During this time, Jinella supported efforts to clean the streets and provided a means for people who were homeless to wash themselves, receive a haircut, and change into clean clothes. Over a few weeks, the health center provided essential items to sustain the effort. Jinella also used the campaign to raise public awareness of the need for personal and environmental hygiene.
The return on this investment was impressive; in January 2020, the typhus caseload fell to ten. By the next month, it dropped to four cases; ultimately reaching zero in March 2020. Since then, there have been no new cases of typhus.
“We found it puzzling. Contrary to the efforts, cases never seemed to slow.”
Around the same time, reports indicated that despite the health center’s best efforts, malaria continued to be on the rise. “We found it puzzling. Contrary to the efforts, cases never seemed to slow down,” says Amal. Confounded, Jinella decided to pause and review its actions against its data.
Again, Jinella turned to its PMT to find answers. The team thoroughly reviewed and analyzed the health data related to malaria and uncovered the mystery: only nine of 169 cases reported from July to December 2020 originated in locations under Jinella’s jurisdiction. Fifty-two percent of cases were from other districts in the Harari region, and 48 percent were from adjacent districts in the Oromia Region.
In total, case data were coming from 12 districts in the two regions, which explained why Jinella’s interventions in its catchment area had failed to reduce the number of malaria cases. This information made it obvious that malaria prevention could be achieved only in coordination and collaboration with stakeholders. Jinella realized it needed to segregate data by source location; and share the data and seek solutions with responsible persons in each location.

Halfway through 2020, Jinella presented its discovery and intervention ideas to the Harari RHB during the regional monthly essential health review meeting, a performance review of the health sector in the Harari region. Jinella and the Harari RHB devised a plan to collaborate with the other woredas and Oromia Region to curb the spread of and ultimately eliminate malaria.
Accordingly, Jinella began sharing data, including data from other districts in the region, via a regional platform. Similarly, the data generated from adjacent districts in Oromia were shared via an existing platform shared between Harari RHB and the Eastern Hararge Zone health departments of Oromia.
Thanks to Jinella’s efforts, malaria reports are now prepared in relation to the case’s origin. This disaggregation has made it possible to reallocate resources to other priority health services. “The fact that we are relieved of the stress of trying to tackle the disease that largely comes from outside our catchment area helped us to refocus our efforts,” says Samiya Baker, health officer at Jinella.
“PMT has become a reliable force behind all these successes. In fact, now it is where it ought to be.”
Jinella’s response to both the typhus outbreak and rise in malaria cases demonstrates its progress in creating a data-driven culture in which actions are based on evidence. Over the last couple of years, the health center also recorded significant improvements in other health services, including family planning and skilled birth attendance. This resounding progress is directly attributed to its optimized PMT, a team that has increased its capacity and strengthened its commitment to review, analyze and translate health data.
Before 2019; however, Jinella had a poor record of data use, and its PMT was ineffective. According to Amal, PMT review meetings were held regularly, but discussions were not translated into action until DUP and the Harari RHB helped the health center build its capacity to generate high-quality data and use it to inform actions. This assistance included on-the-job-training with regional DUP staff to enhance the PMT’s overall performance. Jinella also became one of the health institutions that participated in the Capacity Building and Mentorship Program, which was implemented by DUP, MOH, and local universities. In December 2020, Haramaya University helped organize a week-long training event that was largely credited for promoting a data use culture at Jinella.
Today, the PMT has become the forum that reviews the facility’s performance; identifies and prioritizes health service gaps; and recommends and implements improvement mechanisms. It is where the health center turns to for guidance. “PMT has become a reliable force behind all these successes. In fact, now it is where it ought to be,” says Amal. The health center’s strong family health team and its recognition of high-performing individuals have also contributed to Jinella’s success. To ensure progress and sustainability of its data culture, Jinella has started incentivizing data use behavior. A weekly ceremony recognizes high performers in data use as “Stars of the Week,” and displays their photographs in the health center.
By Benti Ejeta
We strive to build lasting relationships to produce better health outcomes for all.