HIV Self-Testing Comes of Age
April 3rd, 2018 |
It turns out you can teach an old dog new tricks.
The old dog, in this case, is HIV self-testing, a technology first introduced in 2012 and a focus of international public health initiatives ever since. The new trick consists of innovative ways to make HIV self-testing available and attractive to previously hard-to-reach populations.
“We’re finding new people we would not have reached otherwise and they are men,” says Repsina Chintalova-Dallas, a senior technical adviser for the Strengthening High Impact Interventions for an AIDS-free Generation (AIDSFree) Project’s work in HIV testing services.
For men—and other key populations such as young people, health workers, pregnant women, and male partners—HIV self-testing is an “empowering, discreet, and highly acceptable testing option,” says the World Health Organization.[1] A study among men in Zambia, for example, found that adding self-testing to their options boosted the percentage who knew their HIV status. By the end of the study period, 60.4 percent of men with access to self-testing knew their HIV status; the comparable figure among men who were not offered self-testing was 55.1 percent. Self-testing did not seem to have a similar effect among women.
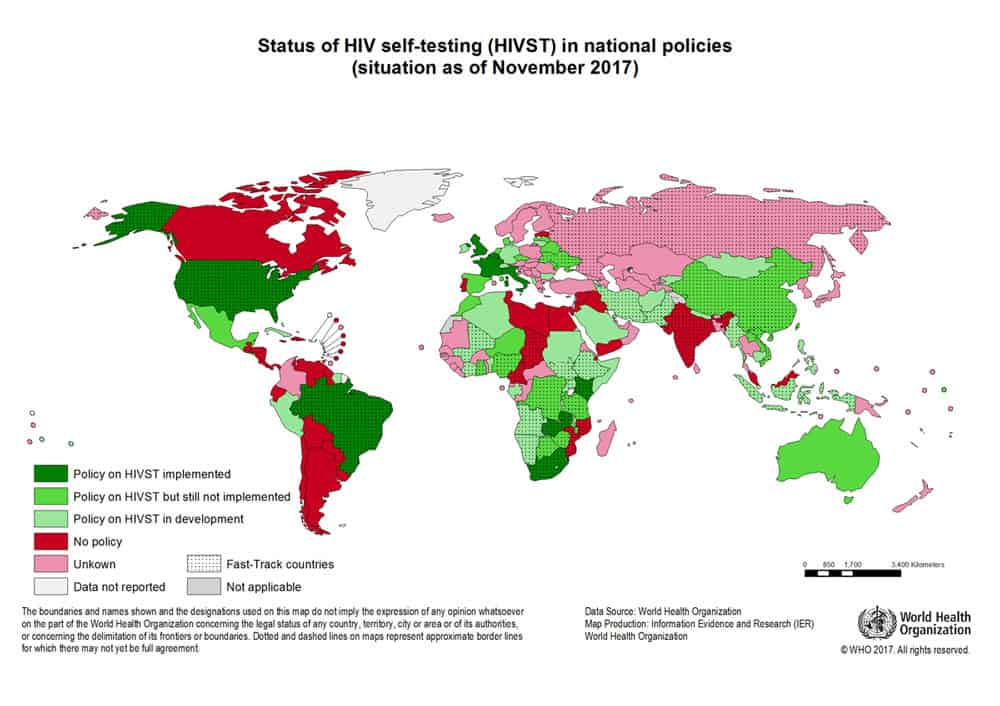
As of November 2017, 41 countries, including most African nations, had HIV self-testing policies or were developing them (see figure below).
In Zambia, JSI is working with peer educators to find effective and acceptable methods of encouraging HIV self-testing among female sex workers.[2] The project compares the direct distribution of an HIV test kit from a peer educator with distribution from a clinic, health post, or similar fixed site.
This year, AIDSFree developed a knowledge base to help country programs expand the reach and effectiveness of their HIV testing services. The knowledge base already has resources dedicated to partner notification. HIV self-testing materials will be posted by late April.
Getting creative
Countries in which AIDSFree works have developed several strategies to make sure a self-test kit is used and to trace its life cycle. These strategies include:
The next step in effective use of HIV self-testing is to understand what happens to the tests after they are distributed. Who is using the kit? How will those who use the kit respond to the result?
It isn’t well understood exactly what happens after someone buys or uses an HIV self-test. “That’s where we need some creative solutions,” says Chintalova-Dallas. “Right now, the only indicator for HIV self-testing is dissemination—how many kits were distributed? That’s not good enough.”
What we do know is that it’s possible to persuade people to opt for an HIV self-test, people who might not otherwise take the test. “The barriers are structural. If you make testing as easy as possible, people will test,” she says.
[1] http://bmjopen.bmj.com/content/bmjopen/7/4/e014780.full.pdf.
[2] World Health Organization. Reaching people with undiagnosed HIV, December 2016. http://apps.who.int/iris/bitstream/handle/10665/251549/WHO-HIV-2016.21-eng.pdf?sequence=1&ua=1
We strive to build lasting relationships to produce better health outcomes for all.